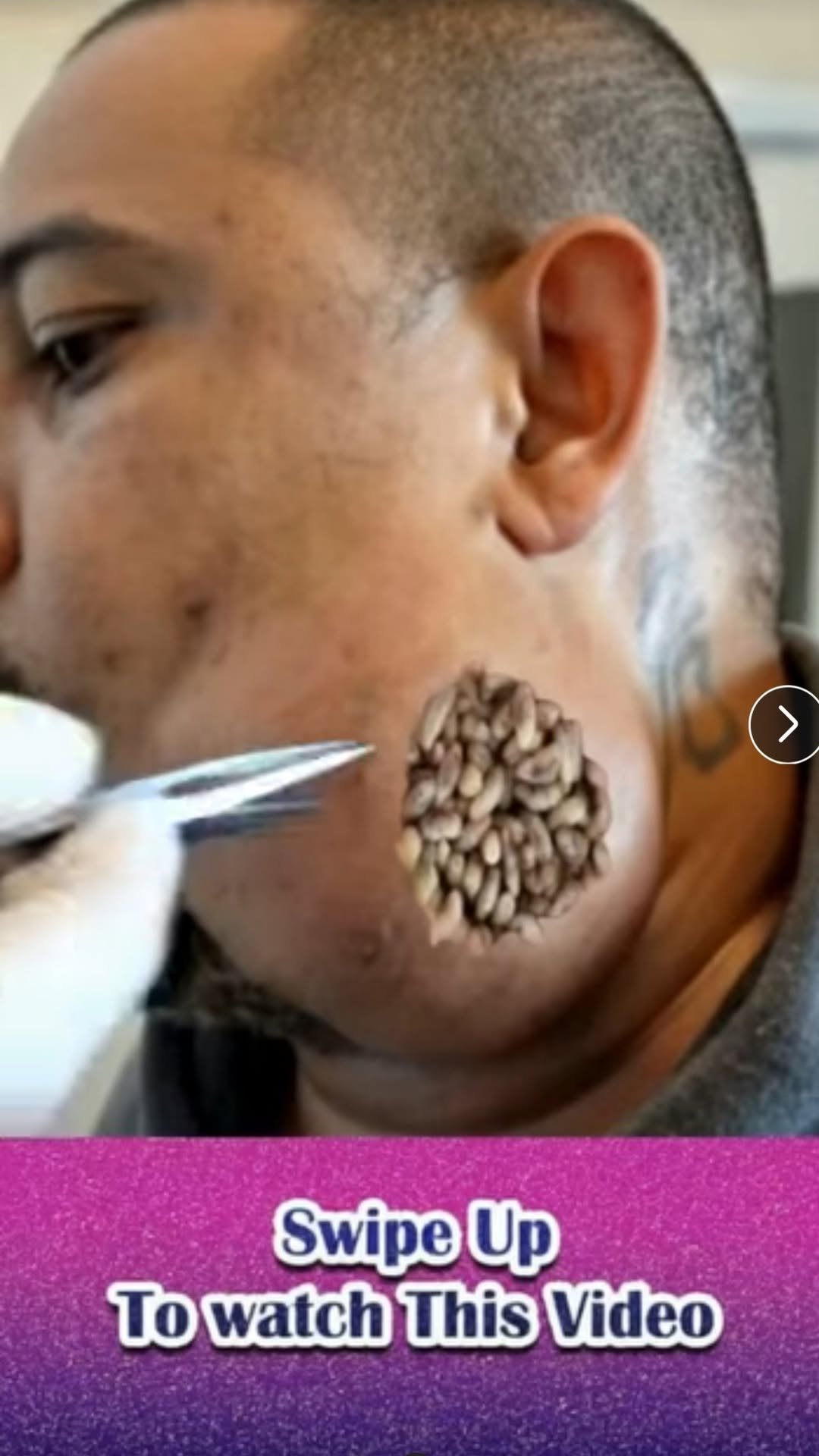
What You’re Seeing: Larvae Infestation (Myiasis)
The image likely depicts a case of nasal myiasis, where parasitic larvae have invaded the nasal cavity. This condition can occur when:
Poor hygiene, open wounds, or infected skin attract flies.
Eggs are laid near moist or inflamed skin (especially in tropical or subtropical environments).
The larvae burrow into the skin or mucous tissue and start feeding on the living or dead tissue.
The result? Swelling, redness, irritation, and sometimes visible movement under the skin or actual emergence of the maggots.
Causes and Risk Factors
While shocking, this condition is medically recognized and occurs more often in:
Rural or underdeveloped areas
People with compromised immunity
Individuals with neglected wounds or poor hygiene
Elderly or bedridden patients
Allergic reactions or bacterial infections often begin the chain—causing scratching, inflammation, or open sores that attract insects. When untreated, bacteria or larvae take advantage of broken skin.
Signs to Watch For
Unusual itching or crawling sensation
Wound that doesn’t heal
Swelling with pus or foul odor
Visible larvae or movement under the skin
If you ever suspect something unusual like this, seek immediate medical attention. This is not a condition you can treat at home.
Prevention Tips
Maintain proper hygiene and treat even small cuts promptly.
Use insect repellent and avoid exposure in fly-prone areas.
Cover wounds and change dressings regularly.
Consult a dermatologist if you notice unusual swelling, boils, or persistent skin irritation.
Final Thoughts
This disturbing image isn’t just a clickbait shock—it’s a real reminder of what happens when infections or allergies go untreated. Don’t ignore what your skin is trying to tell you. Always clean wounds, avoid scratching, and if something seems off—don’t wait.
😱 Stay safe. Stay clean. And don’t let it get this far. 😱
Myiasis (Greek myia “fly” plus -iasis) is an infestation of the skin by developing larvae (maggots) of various of fly species within the arthropod order Diptera. Worldwide, the flies that most commonly cause the human infestation are Dermatobia hominis (human or tropical botfly; see the image below) and Cordylobia anthropophaga (tumbu fly).
 Mature larva of the Dermatobia hominis fly; rows of hooks apparent on its tapered body. Image courtesy of Kenneth E Greer.
Mature larva of the Dermatobia hominis fly; rows of hooks apparent on its tapered body. Image courtesy of Kenneth E Greer.In cutaneous myiasis, the two main clinical types are wound myiasis and furuncular (follicular) myiasis.[1] Other forms include creeping/migratory myiasis and cavitary myiasis of body organs.[2] In nasopharyngeal myiasis, the nose, sinuses, and pharynx are involved. Ophthalmomyiasis affects the eyes, orbits, and periorbital tissue. Intestinal and urogenital myiasis involve invasion of the alimentary tract and the urogenital system, respectively. Hematophagous myiasis, a rare type, is more common in infants younger than 9 months, especially in those living in rural and endemic areas, and the furuncular lesions are usually on the face.[3]
Treatment may involve occlusion or suffocation, irrigation and debridement, surgical removal, or pharmacologic therapy. Patients should be educated about preventive measures to avoid being exposed to or bitten by Diptera flies.

Pathophysiology
Furuncular myiasis
Dermatobia hominis (human botfly)
This type is endemic to tropical southeast Mexico, South America, Central America, and Trinidad. The adult human botfly resembles a bumblebee; it is short-lived, surviving for little more than a week. It does not feed and is infrequently seen.
The life cycle of the botfly is unique, as the female, egg-bearing fly catches a blood-sucking arthropod, usually a mosquito (although 40 other species of insects and ticks have been reported), midflight and attaches her eggs to its abdomen (means of transportation known as phoresy). When the mosquito takes a blood meal from a warm-blooded animal, the local heat induces the eggs to hatch and drop to the skin of the host and enter painlessly through the bite of the carrier or some other small trauma.
Once deposited in the skin, the larvae start out as small and fusiform and later become pyriform to ovoid as they reach full development at lengths of 15-20 mm. They are encircled by several rings of spines. (See the image below.) Eventually, if the cycle is unperturbed, fully-developed larvae emerge from the host in 5-10 weeks and drop to the ground, where they pupate to form flies in 2-4 weeks.[4]
 Mature larva of the Dermatobia hominis fly; rows of hooks apparent on its tapered body. Image courtesy of Kenneth E Greer.
Mature larva of the Dermatobia hominis fly; rows of hooks apparent on its tapered body. Image courtesy of Kenneth E Greer.Cordylobia anthropophaga (tumbu fly)
This type is endemic to sub-Saharan Africa. The adult tumbu fly is about the size of a housefly but stockier. It prefers shade and is most active in the early morning and afternoon. It is attracted by the odor of urine and feces.
The females lay their eggs on dry, sandy soil or on damp clothing hung out to dry. The eggs hatch in 1-3 days and can survive near the soil surface or on clothes for as long as 15 days, waiting for contact with a suitable host. Activated by heat, such as the body heat of the potential host, they are capable of penetrating the unbroken skin with sharp mandibles.[4] They become fusiform to ovoid and reach a length of 13-15 mm. Their larval stage is shorter than that of the human botfly and is completed in 9-14 days.
Creeping (migratory) myiasis
Hypoderma bovis
The adult Hypoderma bovis fly is large and hairy and resembles a bumblebee. The normal hosts for the larvae are deer, cattle, and horses; humans are abnormal hosts, in which the parasite is unable to complete its development. Human infections usually occur in rural areas where cattle and horses are raised.
In animals, the fly attaches its eggs to hairs. The larvae hatch, penetrate the skin, and wander extensively through the subcutaneous tissues, eventually locating under the skin of the back, where they produce the furuncular lesions. In humans, the larvae migrate rapidly (as quickly as 1 cm/h) and erratically through the subcutaneous tissues, producing intermittent painful swelling over a period of months. They may emerge spontaneously from the furuncles or may die within the tissues. In rare cases, larvae may invade the orbit, the pharyngeal region, and the spinal canal.
Gasterophilus intestinalis
The larvae of flies in the Gasterophilus genus are usually gastrointestinal (Gasterophilus intestinalis) or nasal (Gasterophilus nasalis) parasites of horses. In humans, the young larvae burrow in the skin and wander intradermally, creating narrow, tortuous, erythematous, and linear lesions that cause intense pruritus. Lesions usually advance at a rate of 1-30 cm/d.[5] Death of the larvae terminates the infection in 1-2 weeks without sequelae.
Wound myiasis
Wound myiasis may be caused by Cochliomyia hominivorax (New World screwworm) or Lucilia (formerly Phaenicia) sericata (common green bottle fly). The adult flies are rather stocky and metallic blue-green to purplish black in color. The larvae are pinkish, fusiform, and strongly segmented. Female flies deposit the eggs near poorly managed wounds, and the larvae feed on necrotic tissue.[5] Flies may be dispersed by prevailing winds, and infection is often acquired while a person is resting outside during the day or as a consequence of trauma.[3]

Etiology
As noted (see Pathophysiology), myiasis is the consequence of infestation of humans with the larvae of fly species from the order Diptera. More than 100 species from this order have been reported to cause human myiasis. Among the most common are the following:
- D hominis – Furuncular myiasis
- C anthropophaga – Furuncular myiasis
- C hominivorax (America) and Chrysomyia bezziana (Old World screwworm; Africa, Australia, Asia) – Wound myiasis
- H bovis (infested cattle) and G intestinalis (infested horses) – Creeping (migratory) myiasis
- Oestrus ovis (sheep botfly) – Ophthalmomyiasis
Rare cases of oral myiasis caused by Musca domestica (housefly) have been reported.[6]

Epidemiology
In the United States, myiasis is uncommon, and most reported cases involve importation by travelers returning from tropical destinations. However, the incidence has been reported to be increasing among individuals from nonendemic countries who have traveled to tropical destinations or engage in outdoor activities.[7] A study in urban and suburban areas of the United States found an association between cutaneous myiasis and homelessness, alcoholism, and peripheral vascular disease; the fly most commonly identified in that study was L sericata.[1]
Myiasis is a worldwide infestation with seasonal variation. Its prevalence is related to geographic latitude and to the life cycles of the various species of flies. The incidence is higher in the tropical and subtropical areas of Africa[8] and the Americas.[9] Because the flies responsible prefer a warm and humid environment, they are restricted to the summer months in the temperate zones, whereas they live year-round in the tropics.[1] D hominis is endemic to tropical Mexico, South America, Central America, and Trinidad,[10] and C anthropophaga is endemic to sub-Saharan Africa. Ophthalmomyiasis caused by O ovis appears to be most prevalent in Mediterranean countries.[11]
Myiasis may occur at any age. No sex or racial predilection has been shown.

Prognosis
Myiasis is a self-limited infestation with minimal morbidity in the vast majority of cases.[1] The major reasons for treatment are pain reduction, cosmesis, and psychological relief. Once the larva has emerged or has been removed, the lesions resolve rapidly. However, larvae such as those of C hominivorax can infest around orifices of the head and may burrow into brain tissue.[1]
Complications include infections such as cellulitis.[4]
Cases of neonatal fatal cerebral myiasis, caused by the penetration of larva through the fibrous portion of the fontanel, have been reported.[7]

Presentation
History
Often, patients with myiasis have a history of traveling to a tropical country, or the existence of a previous wound is noted. In one study, the average time from exposure to diagnosis was 1.5 months.[12]
Patients complain of lesions resembling boils, usually on exposed areas of the body, such as the scalp, face, forearms, and legs. The lesions can be painful, pruritic, and tender, and patients often have the sense of something moving under the skin. Sometimes, patients also complain of fever or swollen glands.
In the cases of ophthalmomyiasis, patients complain of severe eye irritation, redness, foreign body sensation, pain, lacrimation, and swelling of the eyelids.[13]
In the cases of nasal myiasis, patients present with epistaxis, a foul smell, passage of worms, facial pain, nasal obstruction, nasal discharge, headache, dysphagia, and the sensation of a foreign body in the nose.[14,15]

Physical Examination
Furuncular myiasis
This type of myiasis, which can be caused by either the human botfly or the tumbu fly, causes nonhealing lesions that resemble boils. Whereas myiasis from the tumbu fly occurs on the trunk, thigh, and buttocks, botfly lesions are on the exposed areas of the body, including the scalp, face, forearms, and legs.
A pruritic erythematous papule develops within 24 hours of penetration, enlarging to 1-3 cm in diameter and almost 1 cm in height. These lesions can be painful and tender. Each has a central punctum (see the images below) from which serosanguineous fluid may be discharged. Lesions may become purulent and crusted; the movement of the larva may be noticed by the patient.[1] The tip of the larva may protrude from the central opening (punctum), or bubbles produced by its respiration may be seen.[3] The inflammatory reaction around the lesions may be accompanied by lymphangitis and regional lymphadenopathy.[16]
 Boil-like lesion on toe of a patient with botfly myiasis; the central punctum is apparent. Image courtesy of Kenneth E Greer.
Boil-like lesion on toe of a patient with botfly myiasis; the central punctum is apparent. Image courtesy of Kenneth E Greer. Boil-like lesions on a patient with botfly myiasis; the central punctum is apparent. Image courtesy of Kenneth E Greer.
Boil-like lesions on a patient with botfly myiasis; the central punctum is apparent. Image courtesy of Kenneth E Greer.Wound myiasis
In wound myiasis, the larvae are deposited in a suppurating wound or on decomposing flesh. The diagnosis is obvious when larvae are visible on the surface within or around the wound and more difficult when they have burrowed beneath the surface.[1]
Creeping (migratory) myiasis
Creeping (migratory) cutaneous myiasis may develop in individuals who are exposed to infested cattle or who work with horses. This form of myiasis resembles cutaneous larva migrans, with an apparent tortuous, threadlike red line that ends in a terminal vesicle marking the passage of the larva through the skin. The larva lies ahead of the vesicle in apparently normal skin.[16]
Ophthalmomyiasis externa
Ophthalmomyiasis externa, caused by O ovis, is characterized by conjunctivitis, lid edema, and superficial punctate keratopathy in response to movement of larvae across the external surface of the globe. Larvae may appear within the cornea, the lens, the anterior chamber, or the vitreous body but rarely undergo development once the globe has been entered.[10]
Posttraumatic myiasis
Patients who have sustained facial trauma or have an extensive scalp injury can develop extensive intracranial maggot infestation that may cause meningitis and encephalitis if not properly managed within a reasonable period of time.[17]
Nasal myiasis
In nasal myiasis, examination of the nose (rhinoscopy) reveals an edematous, ulcerated mucous membrane filled with necrotic material and crawling maggots. Patients may have septal perforation, palatal perforation, or both. Erosion of the bridge of the nose and adjacent area of the face can also be seen as well as orbital cellulitis and diffuse cellulitis of the face. In a smaller number of patients, examination reveals extensive ulceration of the tonsils and the posterior pharyngeal wall due to maggots.[15]

DDx
Diagnostic Considerations
Other conditions to be considered include the following:
- Cutaneous leishmaniasis [18]
- Delusions of parasitosis
Differential Diagnoses
Cellulitis
Lymphadenopathy
Tungiasis
Epidermoid Cyst
Insect Bites
Cutaneous Larva Migrans
Workup
Laboratory Studies
The diagnosis of myiasis is typically made by identifying fly larvae or maggots. The exact type of species can be difficult to determine from examination.[4] However, the complete blood count (CBC) may show leukocytosis and eosinophilia.

Imaging Studies
Magnetic resonance imaging (MRI) has been used in a number of cases of cerebral myiasis; breast myiasis; and facial, orbital, and furuncular myiasis. Ultrasonography (US) can also be helpful in establishing the diagnosis and determining the size of the larvae.[19] Computed tomography (CT) has been suggested as well.[20]
In a study by Quintanilla-Cedillo et al, Doppler US with a high-resolution (10-MHz) soft-tissue transducer was used for diagnosis of furuncular myiasis.[21] First, standard-mode US was performed to locate hypoechogenic masses underneath the skin; next, Doppler US was performed, demonstrating circulation of fluid within the parasite as well as showing the number of parasites, their size, and their situation within the lesion. Such findings are especially useful when lesions are still small and look like insect bites; secretion and pain are minimal or absent, and the punctum is almost always absent. In these cases, high-resolution Doppler US proved to be 100% effective in diagnosis.

Procedures
Biopsy is not necessary, but when it is performed, histopathologic findings include an ulcerated epidermis with an inflammatory infiltrate of neutrophils, lymphocytes, giant cells, mast cells, plasma cells, and eosinophils occurring in stages. The larvae can be seen in cross-section.[1,21]

Treatment
Emergency Department Care
Occlusion/suffocation
A noninvasive approach, which involves placing petroleum jelly, liquid paraffin, beeswax or heavy oil, or bacon strips over the central punctum, has been employed to coax the larvae to emerge spontaneously head-first over the course of several hours, at which time tweezers (or forceps) are used to facilitate capture. Enlarging the punctum beforehand may make it easier to remove larvae later as they emerge and is usually necessary for botflies.[22] Anecdotal reports indicate that the larvae generally emerge within 3-24 hours after application of suffocating material.[23,24]
This approach takes advantage of the larva’s oxygen requirements in order to induce it to exit on its own. It is important, however, not to use a covering that is too restrictive (eg, nail polish), because doing so may asphyxiate the larva without causing it to migrate out of the skin. If the larva does asphyxiate, then surgical removal is necessary.
Surgical removal
The skin lesion is locally anesthetized with lidocaine and excised surgically, and the wound is closed primarily. Alternatively, lidocaine can be injected forcibly into the base of the lesion in an attempt to create enough fluid pressure to push the larvae out of the punctum.[25] The larvae are anchored deeply to the subcutaneous tissue by anterior hooklets, and all parts must be removed from the site to prevent a foreign-body reaction.[2] Another surgical approach is to perform a 4- to 5-mm punch excision of the overlying punctum and surrounding skin to gain better access to and visibility of the larvae, which can then be carefully removed with toothed forceps (personal communication, B B Wilson, MD).
The larvae should not be forcibly removed through the central punctum, because their tapered shape with rows of spines and hooks prevents simple extrusion. Furthermore, care should be taken to avoid lacerating larvae during removal, because retained larval parts may precipitate a foreign-body reaction.
After removal of the larvae, antiseptic dressings, thorough cleansing, and debridement are indicated, as well as antibiotics if secondary infection is present.
Ivermectin
An alternative treatment for all types of myiasis is oral ivermectin or topical ivermectin (1% solution), which has proved especially helpful with oral and orbital myiasis.[26] Ivermectin has been found to decrease the associated inflammation and destructive process before debridement.[27] Accordingly, it has been suggested that oral ivermectin should be considered as an option for the treatment of human cavitary myiasis.[28] A case report by Clyti et al described facial furuncular myiasis in an HIV-infected patient who was treated with applications of topical ivermectin solution that killed the larvae and facilitated their extraction.[29]
Management of wound myiasis
Treatment of wound myiasis requires debridement with irrigation to eliminate the larvae from the wound or surgical removal. Application of chloroform, chloroform in light vegetable oil, or ether, with removal of the larvae under local anesthesia, has been advocated for wound myiasis.[1,25]
Surgical removal typically is not required unless requested by the patient, in that the larvae are naturally sloughed within 5-7 weeks.

Complications
Care must be taken to extract the larva whole, otherwise a considerable foreign-body reaction may ensue. Also, in the case of secondary pyogenic infection, appropriate antibiotics should be administered.
Myiasis can be a portal of entry for Clostridium tetani; therefore, vaccination should be considered in affected individuals.[1]

Prevention
Individuals traveling to rural endemic areas should be covered at all times with long-sleeved shirts, pants, and hats. At night, sleeping on raised beds, in screened rooms, or under a mosquito net is appropriate. Insect repellents are also recommended. In areas where tumbu flies are endemic, clothing should be hot-ironed and dried appropriately to remove any residual eggs.[2]
For prevention of wound myiasis, simple antisepsis is usually adequate. Wounds should be cleaned and irrigated intermittently, and proper dressings should be applied. Patients with any type of wound should not be permitted to sleep outside, and if they are sleeping in an indoor or hospital environment, the windows should never be opened unless properly screened.[25]

Consultations
Depending on the location of the larval infestation, consultation with dermatologists (wound and furuncular myiasis), ophthalmologists (ophthalmomyiasis), or otorhinolaryngologists (oral, facial, nasal myiasis) may be warranted.